Targeted Therapy
What is targeted therapy?
Targeted therapy is the use of a drug that specifically attacks the abnormal growth pathway of cancer cells. Normal cells have normal growth pathways and so are not affected by the drug(s).
Each type of targeted therapy attacks different abnormal growth pathways that exist in different types of cancers, thereby interfering with the ability of cancer cells to grow, divide, metastate and communicate with other cells.
There are three major types of targeted drugs:
|
Type |
Drug(trade name) |
|
|
Monoclonal antibody drugs |
Inhibit the HER2 protein on the surface of cancer cells, blocking the signals directing the cells to grow. |
Trastuzumab (Herceptin) |
|
Tyrosine kinase inhibitor |
Inhibit Tyrosine Kinase, an enzyme that activates malignant cellular activities |
Lapatinib(Tykerb) |
|
Inhibitor of mammalian target of rapamycin (mTOR) |
Inhibit P13K/AKT/mTOR pathway and overcome endocrine resistance |
Everolimus (Afinitor) |
How are monoclonal antibody drugs used as targeted therapy?
Antibodies are part of the immune system. Normally, the body creates antibodies in response to an antigen (such as a protein in a germ) entering the body. The antibodies attach to the antigen in order to mark the antigen for destruction by the body's immune system.
In the laboratory, scientists have identified specific antigens in breast cancers and produce monoclonal antibodies as therapeutic drugs to provide specific anti-tumour action within the body. A monoclonal antibody will attach to a matching antigen like a key fitting a lock. This technology allows treatments to target specific cells.
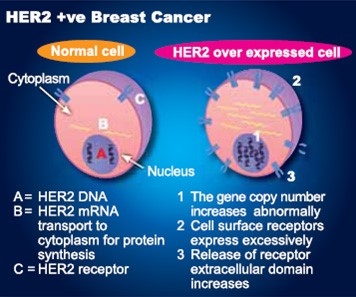
What is HER2 over-expression?
The HER2 (human epidermal growth factor receptor 2) gene, in normal breast cell, is responsible for making the HER2 protein that transmits signals directing cell growth from the outside of the cell to the nucleus inside the cell. In HER2 over-expressed (HER2-positive) breast cancer, there is an increase in the number of copies of the HER2 gene. This results in an increased amount of the HER2 growth factor receptor protein on the tumour cell surface. The over-production of HER2 protein amplifies the growth signal causing the cells to divide, multiply and grow more rapidly. Research has shown that HER2 positive breast cancer is more aggressive than other types of breast cancer.
Is HER2 over-expression inherited?
HER2 over-expression is not inherited from parents while breast cancer genes such as BRCA1 and BRCA2 are inherited.
Why is HER2 testing important?
About 20% of women with invasive breast cancer are HER2 over-expressed (HER2-positive). The monoclonal antibody treatment is applicable only to patients whose breast cancer is identified as HER2 over-expressed (or HER2 positive) in standard testing. Hence, it is very important to find out the cancer’s HER2 status.
Anti-HER2 over-expression drug - Trastuzumab (Herceptin)
What is Trastuzumab (Herceptin)?
The discovery of HER2 gene amplification in breast cancer patients led to the development of Trastuzumab (Herceptin), an artificial monoclonal antibody which acts against the HER2 protein on the surface of breast cancer cells. Trastuzumab (Herceptin) was approved by the FDA in 1998 to be used in first-line treatment in HER2 over-expressed breast cancer patients, and was approved in 2006 for the adjuvant treatment of patients with HER2 over-expressed breast cancer.
According to clinical studies, patients who progress on prior Trastuzumab (Herceptin) treatment would benefit from continuation of Trastuzumab (Herceptin) plus chemotherapy. In addition, publications show that Trastuzumab (Herceptin) could prolong overall survival in patients with brain metastases.
Trastuzumab (Herceptin)
- can be effective in early stage and metastatic HER2 over-expressed breast cancer.
- according to pivotal studies, Trastuzumab(Herceptin) identifies the HER2 breast cancer cells and works by:
-Interfering the growth of cancer cells
-Attracting the body’s own immune cells to help destroy the cancer cells - can work alone or in combination with chemotherapy to destroy HER2 over-expressed cancer cells.
How is Trastuzumab (Herceptin) used?
- Trastuzumab (Herceptin) is administered by slow intravenous infusion.
- It can be given once a week or once every three weeks. It can be administered alone or together with chemotherapy. Prescription is decided by the doctor.
- The dosage depends on the patient’s body weight. The first- time infusion of Trastuzumab (Herceptin) is usually a higher dose (a loading dose).
- Current recommendation on the duration for using Trastuzumab (Herceptin) in early-stage breast cancer is one year.
What are the side effects of Trastuzumab(Herceptin)?
Very common side effects include
- Reactions to the infusion can include fever, nausea, vomiting, headache, diarrhoea, joint pain, muscle pain and rash. These allergic reactions usually occur after the first infusion.
Side effects include: (1-10% patients experience these side effects)
- Influenza-like illness, back pain, weight loss, loss of appetite, dry skin, leucopenia, bone pain.
- Cardiac problems including those without symptoms (reduce heart function) and those with symptoms (congestive heart failure). Trastuzumab and Anthracycline chemotherapy (Epirubicin or Doxorubicin) cannot be given prescribed together because both of them are toxic to the heart. People who have received both treatments are at a higher risk of developing heart problems.
- Trastuzumab (Herceptin) should be withdrawn in any event of a decline in heart function.
- Before and in the process of Trastuzumab treatment, your doctor should monitor your heart performance and conduct an echocardiogram.
- Rare side effects include severe allergic reactions, lung problems, and infusion reactions.
- Side effects vary from person to person. Please consult your doctor with any questions or concern about side effects.
- If you experience swelling, chest pain, or severe shortness of breath, inform your doctor immediately.
Do all HER2 positive patients need Trastuzumab (Herceptin)?
Not all HER2 positive breast cancer patients need Trastuzumab (Herceptin). The HER2 positive patients with recurrent or metastatic disease require anti-HER2 treatment (e.g. Herceptin alone or in combination with hormonal therapy or chemotherapy).
In adjuvant treatment of early-stage HER2 positive breast cancer, anti-HER2 therapy is indicated in intermediate and high-risk patients (patients with lymph node involved or tumour larger than 1 cm). Currently, Herceptin is used together with chemotherapy either in sequence or in combination. There may be a different preference by individual doctors. Duration of Herceptin treatment is one year.
Subcutaneous Herceptin (Herceptin® SC) injections have been available to provide more efficient and convenient method of injection
- It can be given once every three weeks, it can be administered alone or together with chemotherapy
- No need to use loading dose for first injection
- Fixed dose (No Dosage adjustment based on weight)
- It takes only 2-5 minutes to inject
Tyrosine kinase inhibitor drug - Lapatinib (Tykerb)
What is Lapatinib (Tykerb)?
Lapatinib (Tykerb) is a targeted breast cancer therapy with proven therapeutic effects, mainly in HER2 over-expressed breast cancers. The drug, together with the oral chemotherapeutic agent Capecitabine (Xeloda), was approved by the FDA in March 2007.
It is used on refractory HER2 over-expressed breast cancer patients who are previously exposed to chemotherapy and Trastuzumab. It is an orally administrated drug and is found to be effective in disease refractory to Trastuzumab.
How does Lapatinib (Tykerb) work?
- together with Capecitabine, is used on women with HER2 over-expressed, advanced or metastatic breast cancers.
- is a small molecule tyrosin kinese inhibitor which passes through the cell membrane to block the HER2 receptors inside the cell. This stops growth signals from being sent to cancer cells
- works inside the cell (while Trastuzumab works outside the cell).
- is more able to penetrate the blood brain barrier due to its small size. It reaches tumours deeper in the central nervous system than Trastuzumab does. This is important because up to one-third of metastatic HER2 over-expressed breast cancers ultimately develop brain metastases.

How is Lapatinib (Tykerb) used?
- Lapatinib(Tykerb) is a tablet that is taken orally with Capecitabine (Xeloda).
- It is taken daily, before or after meals.
- Please consult your doctor on the dosage and frequency of taking Lapatinib.
What are the side effects of Lapatinib in combination with Capecitabine?
Very common side effects include:
Loss of appetite, diarrhoea, nausea, vomiting, rash, fatigue, poor digestion, dry skin, mucosal inflammation, constipation, abdominal pain, hand-foot syndrome, mucosal inflammation, back pain and insomnia.
Common side effects:(1-10% patients experience these side effects)
- Left ventricular ejection fraction (LVEF) has been reported in approximately 1% of patients.
- LVEF should be evaluated in all patients prior to initiation and continue to be evaluated during treatment to ensure LVEF does not decline to an unacceptable level.
- Paronychia and headache
Other uncommon side effects: (0.1-1% of patients experience these side effects)
Interstitial lung disease, inflammation of lung tissues and liver damage.
Not everyone taking Lapatini (Tykerb) experiences side effects. Please ask your doctor for further information.
Inhibitor of mammalian target of rapamycin (mTOR)-Everolimus (Afinitor)
What is Everolimus (Afinitor)?
For postmenopausal women with HR+ metastatic breast cancer, hormonal treatment is the most common treatment choice. Over time, however, this therapy can stop working and the cancer can come back or spread to somewhere new in the body. When this happens, the cancer is said to develop “resistance” to hormonal treatment. One of the explanations of hormone resistance is activation of the mTOR growth pathway bypassing the blockade induced by hormone. The use of a mTOR inhibitor (eg. Everolimus) together with a hormone agent (eg. exemestane) can be useful in this situation.
A clinical study has shown that patients who received Everolimus (Afinitor) in combination with exemestane had more than double the time of progression-free survival (a term that measures the amount of time without tumours growing or spreading), compared to patients who took only exemestane.
When breast cancers develop resistance to hormonal therapy, PI3K/AKT/ mTOR pathway will be activated by passing the growth signal transduction block in the hormone pathway. Everolimus (Afinitor) can overcome endocrine resistance by simultaneous blockade of both the hormone and mTOR pathways.
How does Everolimus (Afinitor) work?
- Works together with hormone therapy in a new way to overcome endocrine resistance.
- When prescribed with a hormonal anticancer therapy, exemestane, can increase the time that exemestane will be effective in keeping the disease from progressing.
- Combined with exemestane enhances the benefit of taking exemestane alone.
How is Everolimus (Afinitor) used?
- Everolimus (Afinitor) (10mg) is given with exemestane (25mg) to treat HR+ advanced breast cancer.
- Everolimus (Afinitor) and exemestane are taken orally, once a day, at the same time every day either consistently with or without food.
- Swallowed with a full glass of water. Do not chew or crush the tablets.
- Do not drink grapefruit juice or eat grapefruit while taking Everolimus (Afinitor).
What are the side effects of Everolimus (Afinitor)?
Common side effects to monitor:
- Mouth ulcers and sores
- Feeling weak or tired
- Diarrhoea
- Rash, dry skin, and itching
- Swelling of arms, hands, feet, ankles, face or other parts of the body
- Abnormal taste
- Headache
- Nausea and vomiting
- Nose bleeds
- Loss of appetite
Serious side effects to watch for:
- Lung or breathing problems (cough, coughing up blood, chest pain, shortness of breath)
- Fever, chills, or other signs of infection
Advise your doctor right away if you have any of the above side effects or symptoms, early treatment can keep side effects from getting worse.
Pertuzumab (Perjeta)
What is Pertuzumab (Perjeta)?
PERJETA is a US Food and Drug Administration and Hong Kong Department of Health approved treatment for HER2-positive metastatic breast cancer. It is indicated for
- Use in combination with trastuzumab and docetaxel in adult patients with HER2-positive metastatic or locally recurrent unresectable breast cancer, who have not received previous anti-HER2 therapy or chemotherapy for their metastatic disease.
- In combination with trastuzumab and chemotherapy for the neoadjuvant treatment of adult patients with HER2-positive, locally advanced, inflammatory, or early-stage breast cancer at high risk of recurrence.
Pertuzumab (Perjeta) is proven to prolong the median progression-free survival and median overall survival for HER2-positive metastatic breast cancer patient.
In a clinical study, Pertuzumab (Perjeta)+Trastuzumab (Herceptin) +docetaxel are compared with Trastuzumab (Herceptin) + docetaxel for HER2-positive metastatic breast cancer patients.
The result showed that Perjeta group can prolong the median progression-free survival by 6 months (18.5 months vs 12.4 months) and also increase the median overall survival by 15.7 months (56.5 months vs 40.8 months) compared with Trastuzumab (Herceptin) group.
How does Pertuzumab (Perjeta) work?
HER2 works by sending signals that tell cells to grow and divide. One way that HER2 can send signals is by pairing with other HER receptors. This process is called dimerization HER2.
Pertuzumab (Perjeta) is monoclonal antibody and combined used with Trastuzumab (Herceptin) and docetaxel for HER2-positive metastatic breast cancer.
- PERJETA and Herceptin both target HER2 but work in different ways
- PERJETA is thought to block one method of signalling so that certain receptors are unable to pair (dimerization) with HER2
- Together, PERJETA and Herceptin are thought to create a stronger blockade against HER2 signals, helping to slow down cancer cell growth.
How is Pertuzumab (Perjeta) used?
- Pertuzumab (Perjeta) is administered by slow intravenous infusing.
- It can be given once every three weeks.
- Combination used with Pertuzumab (Perjeta), Trastuzumab (Herceptin) and docetaxel.
What are the side effects of Pertuzumab (Perjeta)?
Common side effects
- Diarrhoea
- Hair loss
- Low levels of white blood cells with or without a fever
- Nausea
- Feeling tired
- Rash
- Damage to the nerves (numbness, tingling, pain in hands/feet)
Trastuzumab emtansine (KADCYLA®)?1
What is Trastuzumab emtansine (KADCYLA®)?1
KADCYLA is the first HER2-targeted treatment of its kind for metastatic breast cancer. It is made up of 2 cancer-fighting drugs in 1:
- The monoclonal antibody trastuzumab (the same monoclonal antibody in Herceptin®)
- A chemotherapy drug DM1
How is Trastuzumab emtansine (KADCYLA®) thought to work?1
- The monoclonal antibody part of KADCYLA (trastuzumab) is made to find HER2-positive cells and attach to them. It tells the cells to stop growing and tells the body’s immune system to destroy them.
- The chemotherapy part of KADCYLA (DM1) further destroys the cancer cell by inhibiting the aggregation of microtubules.
KADCYLA is approved to treat HER2-positive breast cancer that has spread to other parts of the body (metastatic breast cancer) after prior treatment with trastuzumab (Herceptin®) and a taxane.
How do I take KADCYLA®?1
Like many cancer medicines, KADCYLA® is given by intravenous (IV) infusion. KADCYLA® is given in your doctor’s office or at a hospital or infusion centre. You will get an infusion of KADCYLA once every 3 weeks.
The first infusion will last 90 minutes. During and after the first infusion, caretakers will observe if any infusion reaction occurs. If the patient feels well after the first infusion, the following infusions will shorten to 30 minutes.
What are the most common side effects of KADCYLA®?1
The most common side effects seen in people taking KADCYLA were:
- Tiredness
- Nausea
- Pain that affects the bones, muscles, ligaments, and tendons
- Bleeding
- Low Platelet count
- Headache
- Liver problems
- Constipation
- Nosebleeds
Special thanks to Dr. Kwan Wing Hong and Dr. Lawrence Li Pui Ki for editing
12/2016

